Sir Alexander Fleming's discovery of penicillin in 1928 was so revolutionary that the Scottish physician received a Nobel Prize, a knighthood, and a spot on TIME's list of the most important people of the 20th century. Antibiotics have since saved millions of lives, but now the power of these miracle drugs is in serious jeopardy.
The Centers for Disease Control released a new Vital Signs report this week detailing the terrifying spread of "nightmare bacteria," infection-causing germs resistant to all currently available antibiotics.
Out of 5,776 samples, federal health officials identified rare antibiotic-resistant genes in more than 200 of them in 27 states across the country. Even more alarming, they discovered that one out of every four samples tested showed the capability of spreading resistance to other bacteria.
"I was surprised by the numbers we found," Dr. Anne Schuchat, principal deputy director of the CDC, told CNN. "Two million Americans get infections from antibiotic resistance, and 23,000 die from those infections each year."
How Antibiotic Resistance Works
Antibiotic resistance developed in response to the increased and continued use of antibiotics. As the word literally means "against life" in Greek, these drugs kill both bad bacteria causing illness as well as good bacteria protecting the body from infection. However, bacterium can "learn" to defend against antibiotics it's seen before, or even similar ones. By resisting the drug, the bad bacteria not only survives, but the dearth of good bacteria allows it to proliferate. The drug-resistant bacteria then takes over, and even passes on its superior defense mechanisms to other germs.
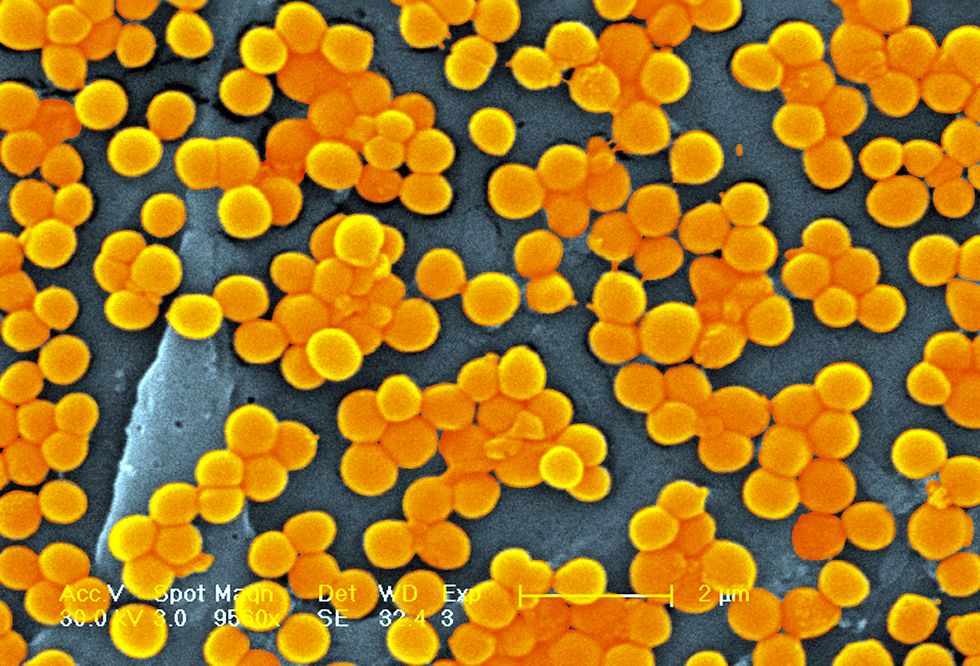
Doctors have known about this problem for decades, and you've probably heard of MRSA (methicillin-resistant staph aureus) before — the strain that resists all drugs in the penicillin family. Another group called CRE (Carbapenem-resistant enterococci) can withstand the most powerful antibiotics available, according to ABC News.
Other bacteria can resist multiple classes of drugs. Since they're "virtually untreatable," as many as half of patients infected with nightmare bacteria die, according to Dr. Schuchat.
In 2014, the World Health Organization stated that a "post-antibiotic era — in which common infections and minor injuries can kill — far from being an apocalyptic fantasy, is instead a very real possibility for the 21st century."
What's Being Done About It
While the results definitely sound scary, this new report comes as a direct result of increased funding to the CDC to prevent the spread of resistant bacteria. In January 2017, the organization launched a new nationwide network of labs that identify problematic pathogens before big outbreaks hit, NPR reports. When they detect unusual germs (usually in a hospital or healthcare facility), officials work to contain the infection and prevent its spread to others.
Physicians can also look to use antibiotics more effectively. Doctors prescribe unnecessary antibiotics at least 30% of the time, according to the CDC. For example, many patients insist on receiving the treatment for the common cold, even those most of these infections come from viruses. Antibiotics only treat bacteria and don't affect viruses like the common cold or the flu.
There's room for improvement outside of the medical field as well. The CDC says that everyone should always practice good hygiene, including washing hands frequently and keeping cuts clean until healed. When you see doctors, inform them if you've received health care in another country or facility, and talk to them about preventing infections, caring for chronic conditions, and receiving recommended vaccines. Taking these basic steps (don't skip the soap!) can help protect you against potential pathogens, whether they're the nightmare variety or not.
Follow Delish on Instagram.